
What is viral meningitis and what causes it?
Coxsackie or Echovirus groups of enteroviruses are the most common cause of viral meningitis. Most infections produce no symptoms, or mild symptoms such as sore throats, colds and flu-like illnesses. Some of them may also cause stomach upsets and diarrhoea. Enteroviruses mostly affect children, who are the main transmitters of these viruses.
Can viral meningitis clear on its own?
Viral meningitis is usually mild and often clears on its own. Most cases in the United States are caused by a group of viruses known as enteroviruses, which are most common in late summer and early fall. Viruses such as herpes simplex virus, HIV, mumps virus, West Nile virus and others also can cause viral meningitis.
What are the dangers of vaping?
Vaping or inhaling aerosolized agents not only irritates the mouth and nasal cavity, but has been known to increase nose bleeds, cause mouth sores, dry mouth, and even loss of taste, Dr. Stiehm points out. Among experienced vapers, the amount of nicotine in the blood rivals the amount they would get from smoking a cigarette, says Dr. Stiehm.
Can herpes cause meningitis?
Major members of the family Herpesviridaethat can cause meningitis include human herpesvirus 1 and 2 (HSV-1 and HSV-2), varicella-zoster virus (VZV), and Epstein-Barr virus (EBV) [82]. The major neurological consequences of HSV are encephalitis and meningitis [83, 84].
What Causes Viral Meningitis?
There are a number of viruses that can cause meningitis. They include: 1. Enteroviruses 2. Herpes simplex virus 1 and 2 3. Varicella zoster virus,...
What Are Other Causes of Viral Meningitis?
Certain insects can also transmit viruses that cause meningitis, such as: 1. West Nile virus from mosquitos in certain parts of the Americas, Afric...
Is Viral Meningitis Contagious?
Yes, but it’s unlikely to spread. While the viruses that cause the disease are generally easily passed between people, viral meningitis itself is n...
How Long Does Viral Meningitis Last?
Most cases go away on their own within 7 to 10 days. (1) Sometimes recovery can take a few months; this is most likely if the meningitis is caused...
Is Viral Meningitis fatal?
It can be, but according to the National Meningitis Association, it’s not as deadly or incapacitating as bacterial meningitis. (7)It can be deadly...
Can You Get Viral Meningitis More Than once?
Yes. But it is very rare for a person to have two or more episodes of meningitis, because most people develop immunity to the virus that caused the...
How Is Viral Meningitis Treated?
If a person is acutely ill, antibiotics will be administered while waiting for test results to confirm whether the illness is bacterial meningitis,...
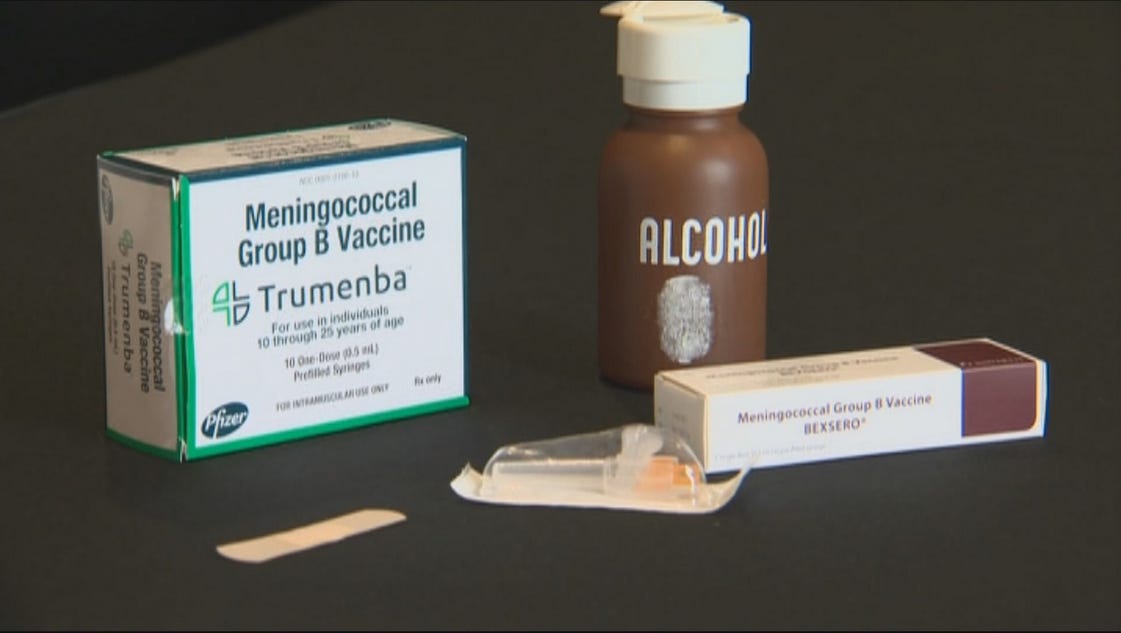
How Can You Prevent Viral Meningitis?
Vaccines can prevent some types of viral meningitis, though this doesn't include meningitis caused by enteroviruses.In this case, avoiding close co...
Can viral meningitis be prevented?
Most causes of viral meningitis are not preventable, although a good general precaution against viral meningitis is attention to handwashing since enteroviruses in particular usually enter the body via the hand to mouth route. Immunisation against mumps and measles (MMR) is offered to children at 12-13 months and 3 years of age as part of the routine childhood immunisation schedule. Immunisations are also available for some Flaviviruses such as tick-borne encephalitis and Japanese encephalitis, and are recommended for travellers to areas where the risk of these infections is high.
What is the cause of meningitis in adults?
Herpes viruses are the other common cause of viral meningitis in adolescents and adults in developed countries [2]. Herpes viruses include the herpes simplex viruses (HSVs) and varicella zoster virus – the same virus that causes chickenpox and shingles. HSVs can cause meningitis or encephalitis (inflammation of the brain itself, ...
What are the diseases that affect wild animals?
Flaviviruses. These viruses normally affect wild animals such as birds or rodents and are carried by mosquitoes or ticks. Some of these viruses such as West Nile virus, Japanese B encephalitis and tick-borne encephalitis can cause meningitis or encephalitis in humans but this is not a problem in the UK and Ireland.
What is the most common cause of meningitis?
Coxsackie or Echovirus groups of enteroviruses are the most common cause of viral meningitis. Most infections produce no symptoms, or mild symptoms such as sore throats, colds and flu-like illnesses. Some of them may also cause stomach upsets and diarrhoea.
How do you get HSV-1?
Transmission is via contact with an infected area of the skin when the virus is active. HSV-1 is usually acquired orally during childhood and about 6 out of 10 people in the UK carry it. HSV-2 is primarily a sexually transmitted infection and is carried by about 1 in 10 of the UK population[3]. Many people harbour HSV without ever knowing they have it. Since they can transmit the virus without having symptoms, infection can be spread unknowingly to contacts. The timing of transmission is unpredictable, so genital herpes infection (and herpes meningitis) can appear even after many years in a monogamous relationship.
What is a lumbar puncture?
This is when a sample of cerebrospinal fluid (CSF) is taken from the spinal canal (the passageway through the back bones which contains the spinal cord). The sample of CSF will be examined and then sent for further laboratory testing.
Can meningitis cause short term memory loss?
Most people recover with no noticeable effects, however recent studies have found that some patients with viral meningitis may develop short-term memory loss and attention deficits [5-6]. There is also some evidence that children who have viral meningitis under 1 year of age, may develop subtle neurological problems later in life [7].
What Causes Viral Meningitis?
There are a number of viruses that can cause meningitis. They include:
Is Viral Meningitis Contagious?
Yes, but it’s unlikely to spread. While the viruses that cause the disease are generally easily passed between people, viral meningitis itself is not very easily passed between people. When it is, it happens mostly between people who are in regular, close contact. (1, 5)
How Long Does Viral Meningitis Last?
Most cases go away on their own within 7 to 10 days. (1) Sometimes recovery can take a few months; this is most likely if the meningitis is caused by West Nile virus or lymphocytic choriomeningitis virus. ( 6)
Can You Get Viral Meningitis More Than Once?
Yes. But it is very rare for a person to have two or more episodes of meningitis, because most people develop immunity to the virus that caused their disease.
How Is Viral Meningitis Treated?
If a person is acutely ill, antibiotics will be administered while waiting for test results to confirm whether the illness is bacterial meningitis, which requires immediate treatment.
How Can You Prevent Viral Meningitis?
Vaccines can prevent some types of viral meningitis, though this doesn't include meningitis caused by enteroviruses.
How long does it take for Mollaret meningitis to subside?
( 8) These illnesses last about two to five days, then subside on their own.
What is the Nigrovic model?
Development and validation of a multivariable predictive model to distinguish bacterial from aseptic meningitis in children in the post-Haemophilus influenzae era. Pediatrics. 2002 Oct;110(4):712-9. [PubMed: 12359784]
What is the pathology of meningitis?
Meningitis is an inflammatory pathology of the meninges surrounding the brain.[3] Viruses can reach the meninges in a variety of ways, including spread via the bloodstream, retrograde spread from nerve endings, and reactivation from a dormant state within the nervous system. [3][4] As a virus reaches the central nervous system (CNS) and spreads through the subarachnoid space, it causes an inflammatory response resulting in meningitis.[8] Encephalitis occurs when there is inflammation of the brain parenchyma and is associated with a worse prognosis. [1][3] The mumps virus is highly neurotropic and can directly infect the epithelium of the choroid plexus.[4] Enteroviruses replicate outside the CNS and reach the CNS via hematogenous spread. [8]
What is the most common cause of meningitis?
Enteroviruses rank as the most common cause of viral meningitis in many places in the world, with up to 12 to 19 cases per 100000 population annually in some high-income countries.[7] WNV, which is spread by mosquitoes, can cause meningitis and encephalitis. It is now endemic in North America and carries a 4 to 13% fatality rate. Mortality is higher in patients who are elderly, immunosuppressed, or have diabetes.
What is viral meningitis?
Viral meningitis is the inflammation of the meninges caused by a virus. It is most common in young children but is seen across all age groups. This activity reviews the evaluation and management of viral meningitis and explains the role of the interprofessional team in evaluating and treating patients with viral meningitis.
What can PCR test do to a virus?
Utilization of PCR tests to diagnosis viruses such as enterovirus, HSV, and VZV can decrease the length of stay and reduce antibiotic administration. [1]
What is the Creative Commons 4.0 license?
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
What is EV-D68?
Enterovirus D68 (EV-D68) is the most common member of the species Enterovirus Dfound to be associated with the development of aseptic meningitis. EV-D68 can cause CNS complications in children, commonly meningitis and flaccid paralysis [72]. The pathogenesis of EV-D68 is quite different from that of other enteroviruses, since it is a respiratory virus. As the virus enters the upper respiratory tract (URT), it binds to the N-acetylneuraminic acid α2,6-galactose receptor found on the surface of the epithelial cells. This receptor is predominant in the upper respiratory tract (URT) [73], which could explain the limited spread of the virus and its rare progression to neurological complications, such as meningitis. It has also been found that the virus binds to the cellular receptor ICAM-5/telencephalin, which is expressed in dendrites and some neurons, to enter the cell [74, 75]. In addition, EV-D68 can reach the CNS through binding to the functional receptors of the olfactory nerve in the nasal cavity [76]. The neuropathogenesis of EV-D68 and its ability to infect neuron cells may highlight the potential link between EV-D68 infection and aseptic meningitis.
What is the coxsackie virus?
Coxsackievirus B, a member of the species Enterovirus B , is known to cause meningitis and other neurological disorders [63]. A proposed route of coxsackievirus entry to the CNS is through infected mononuclear cells (Mac-3) that can penetrate the BBB and invade the choroid plexus epithelium, allowing the spread of the virus into the CNS [64, 65]. This leads to the activation of extracellular signal-regulated kinases 1 and 2 (ERK-1/2), subsequently promoting viral replication inside leukocytes, mainly T cells [66]. Another study demonstrated that this virus replicates in monocytes, T cells, and B cells during the viremia phase and that the level of susceptibility of immune cells to infection determines the severity of secondary organ damage [67], such as causing severe meningitis after reaching the CNS. Moreover, analysis of brain tissues obtained from mice born to mothers inoculated with coxsackievirus B4 showed signs of meningitis and accumulation of immune cells (mainly T cells) and increased secretion of inflammatory cytokines and chemokines (IL6, TNF-α, IFNα and MCP-1) [68]. Echoviruses, such as E-6, E-9, E-11, E-13, E-19, and E-30 also belong to the species Enterovirus Band are commonly known to be associated with viral meningitis in children [69]. Different studies have shown that echoviruses use a special type of integrin (α2 β1, very late antigen 2 [VLA-2]) and decay-accelerating factor as receptors to infect host cells to cause meningitis and febrile illness [70]. In a study by Lee et al. on aseptic meningitis, it was found that E-30 affects the triple functional domain (TRIO) protein, leading to neural damage (Fig. (Fig.2)2) [71]. E-30 can cause neural damage by modulating the function of the TRIO protein. In the first pathway, the virus affects the function of guanine exchange factor domain 2 (GEFD2), which results in the activation of Ras homology family member A (RhoA), a GTPase signaling protein. This activates both the ROCK and MLC signaling pathways. This cascade of events leads to actin formation and elevation of the nitric oxide level, resulting in CNS complications [71].
What are the three membranes of the brain?
Meningitis is an inflammation that affects the three protective membrane layers that cover the brain and spinal cord, called the meninges [1]. The outer layer of the meninges is called the dura mater, followed by the arachnoid mater and the pia mater. The two inner layers (arachnoid and pia mater) are also called the leptomeninges and are separated by the subarachnoid space, which contains cerebrospinal fluid (CSF) [2]. Aseptic meningitis, also known as slow viral disease, became an area of interest at the beginning of the 1950s, when it was considered a potential model for chronic nervous system diseases [3]. Bacteria are the most common causative agents of meningitis. However, viruses, fungi, and non-infectious agents such as drugs can also induce meningitis [2]. Pathogens can reach the CSF through hematogenous spread by two main mechanisms: 1) by infecting immune cells, which in turn carry the pathogen to the nervous system, and 2) by crossing blood capillaries and entering the CSF as free pathogens [4]. The term aseptic meningitis is used to describe meninges inflammation that is caused by pathogens other than pus-producing bacteria [5]. Viral meningitis is the most common type of aseptic meningitis and usually affects young children [1]. Enteroviruses (EVs) are the most common causative agents of viral meningitis, with an estimated 75,000 new cases annually in the United States [6]. Here, we provide an overview of viral meningitis and its most common causative agents and their pathogenesis. We also discuss epidemiological aspects, diagnosis, and clinical manifestations of the disease.
What are the causes of meningitis?
Major members of the family Herpesviridaethat can cause meningitis include human herpesvirus 1 and 2 (HSV-1 and HSV-2), varicella-zoster virus (VZV), and Epstein-Barr virus (EBV) [82]. The major neurological consequences of HSV are encephalitis and meningitis [83, 84]. All of these viruses are known to cause meningitis and can establish a latent infection in neurons, which can be reactivated [82]. Four glycoproteins in HSV-1 and HSV-2 are important for viral entry (gB, gD, gH, and gL); however, cell binding is mediated by only two glycoproteins, gB and/or gC, that bind to cell-surface heparan sulfate [82]. Three known cellular receptors have been identified for HSV: 1) herpesvirus entry mediator (HVEM), 2) members of the immunoglobulin superfamily, and 3) heparan sulfate generated by certain isoforms of 3-O-sulfotransferases [82]. HVEM is present on the surface of various cell types, including epithelial cells and neurons. Accordingly, viral entry through this receptor is suggested in meningitis. EBV pathogenesis starts when the virus infects oropharyngeal epithelium cells. It then spreads to the lymphoid tissue and infects lymphoid cells, mainly B cells. In the infected B cell population, the virus can be latent or, less frequently, lytic. In the latent stage, the virus mainly expresses EBNAs (Epstein-Barr nuclear antigens) and LMPs (latent membrane proteins) [85]. The virus can also infect the endothelial cells of blood vessels in the brain, causing latent infection. When the brain undergoes stress, the virus can be activated and the expression of different cytokines and chemokines, such as IL-1, TNF-α, IL-12 and IL18 increases, resulting in an inflammatory response [86].
How to diagnose meningitis?
Diagnosis of meningitis starts with a physical examination and a review of the patient's health history for any of the signs mentioned above. A recent and less recognized physical examination technique that has been developed to assess meningeal irritation is known as jolt accentuation of headache. A systematic review done by Iguchi and colleagues showed that jolt accentuation can be used in emergency settings to exclude meningitis. However, the pooled sensitivity and specificity of this test (65.3%, 70.4% respectively) are considered low, and more research is needed to assess its usefulness [32]. To test for etiological agents, a lumbar puncture and collection of CSF is needed. The procedure is performed while the patient is in a lying or sitting position, and a hollow needle is injected into the subarachnoid space between vertebrae L3, L4 or L5, where the CSF is aspirated [33]. The CSF is then tested to determine red blood cell and leukocyte count as well as the glucose and protein levels. The cell counts typically help in differentiating the different types of meningitis. For instance, a high WBC count (≥ 500 cells/μl) with a large proportion of neutrophils (>80%) is usually observed in bacterial meningitis. Furthermore, in bacterial meningitis, the CSF glucose level typically does not exceed (300 mg/dL), but a decreased glucose CSF/blood ratio (< 0.4), and an elevated protein level (1 g/l) are indications of bacterial meningitis [2]. In addition, the concentration of lactic acid (≥ 4.2 mmol/l) can be used to differentiate between viral and bacterial meningitis with 100% specificity [34]. Gram staining and bacterial culture are the key diagnostic tools for identifying bacterial infections [2], and viral meningitis is suspected when Gram staining and culture of CSF are negative. In viral meningitis, the WBC count typically ranges between 80 and 100 cells/μl (pleocytosis), with a large proportion of lymphocytes (>80%) [21]. Also, glucose and protein levels usually remain normal [35]. Pleocytosis generally is considered an important criterion for diagnosis of viral meningitis. However, a number of studies have shown that pleocytosis is often not observed in EV meningitis cases involving infants (38%) or children (39%), or when a lumbar puncture is performed at an early stage of disease [36, 37]. The reason for this is not known, but it might be explained by the immaturity of the immune system in young children [38]. The presence of neutrophilic pleocytosis is usually indicative of bacterial meningitis rather than viral meningitis. However, it has been found that 25% of patients with CNS abnormalities caused by viral agents have neutrophilic pleocytosis [39]. Moreover, a study showed that 47% of study subjects with enteroviral meningitis had neutrophilic pleocytosis [40].
What are the different types of arboviruses?
These include members of the families Flaviviridae(e.g., West Nile virus [WNV]), Togaviridae(e.g., Eastern equine encephalitis virus), and Peribunyaviridae(e.g., La Crosse virus). Most of these viruses are zoonotic and are transmitted to humans through arthropods such as mosquitoes, ticks, and sandflies. The most important arbovirus associated with CNS complications is WNV [94]. In the case of the arboviruses, viral entry can occur through skin bites from infected arthropods, which results in regional lymph node infection, viremia, and spread to the CNS, leading to meningitis [29].
What is the West Nile virus?
West Nile virus commonly causes West Nile neuroinvasive disorders (WNNDs), such as aseptic meningitis, paralysis, and encephalitis. The pathogenesis of the virus depends mainly on the replication of virus in the host's lymph nodes and skin keratinocytes [95], resulting in primary viremia. The virus can then spread to secondary locations such as CNS after penetrating the BBB [96]. Infection of the CNS by WNV activates Toll-like receptor 3, increases the concentration of TNF-α and other pro-inflammatory factors, which in turn increases the permeability of the BBB and leads to neural death [96]. Therefore, WNV infection can trigger the development of various neurologica1 complications, including meningitis.
How long does it take for meningitis to heal?
Most people who have viral meningitis recover within a few weeks. Occasionally, recovery can take months, as sometimes occurs when meningitis is caused by West Nile virus or lymphocytic choriomeningitis virus.
What is the term for inflammation of the layers of tissue that cover the brain and spinal cord?
Images (1) Lab Test (0) Tables (0) Videos (0) Viral meningitis is inflammation of the layers of tissue that cover the brain and spinal cord (meninges) and of the fluid-filled space between the meninges (subarachnoid space) when it is caused by viruses. Viral meningitis usually begins with symptoms of a viral infection such as fever, ...
What does it mean when antibodies to a virus increase?
An increase in the level of antibodies to a particular virus indicates that the virus caused a recent infection and so probably was the cause of recent meningitis.
What is aseptic meningitis?
Aseptic meningitis refers to meningitis that is caused by anything other than the bacteria that typically cause meningitis. Thus, aseptic meningitis can include meningitis caused by drugs, disorders that are not infections, or other organisms (such as the bacteria that cause Lyme disease or syphilis ).
What is a spinal tap?
Viral meningitis is more likely when the symptoms are less severe. A spinal tap (lumbar puncture) is done to obtain a sample of cerebrospinal fluid.
What does it feel like to have a viral infection?
Viral meningitis usually begins with symptoms of a viral infection such as fever, a general feeling of illness, headache, and muscle aches. Later, people develop a headache and a stiff neck that makes lowering the chin to the chest difficult or impossible.
Where is the subarachnoid space?
The subarachnoid space is located between the middle layer and the inner layer of the meninges, which cover the brain and spinal cord. It contains the cerebrospinal fluid, which flows through the meninges, fills the spaces within the brain, and helps cushion the brain and spinal cord. Viral meningitis is the most common cause of aseptic meningitis.
What causes viral meningitis?
According to the National Institute of Neurological Disorders and Stroke (NINDS), viral meningitis is most frequently caused by enteroviruses, a group of viruses that can enter the body through the mouth and make their way to the brain and surrounding tissues, where they multiply.
How is viral meningitis diagnosed?
To diagnose viral meningitis, doctors often use a lumbar puncture, or spinal tap, in which a needle is inserted into the lower spine and a small amount of cerebrospinal fluid is drawn for testing.
What causes meningitis in animals?
Parasites can cause a rare type of meningitis called eosinophilic meningitis. Parasitic meningitis can also be caused by a tapeworm infection in the brain (cysticercosis) or cerebral malaria. Amoebic meningitis is a rare type that is sometimes contracted through swimming in fresh water and can quickly become life-threatening. The main parasites that cause meningitis typically infect animals. People are usually infected by eating foods contaminated with these parasites. Parasitic meningitis isn't spread between people.
What is the most common cause of meningitis in the US?
Viral meningitis is usually mild and often clears on its own. Most cases in the United States are caused by a group of viruses known as enteroviruses, which are most common in late summer and early fall. Viruses such as herpes simplex virus, HIV, mumps virus, West Nile virus and others also can cause viral meningitis.
How old is the most likely age to get meningitis?
Age. Most cases of viral meningitis occur in children younger than age 5. Bacterial meningitis is common in those under age 20.
What is the name of the membrane that protects the brain and spinal cord?
Close. Meningitis. Meningitis. Meningitis is an infection and inflammation of the fluid and three membranes (meninges) protecting your brain and spinal cord. The tough outer membrane is called the dura mater, and the delicate inner layer is the pia mater.
How long does it take for meningitis to kill?
Bacterial meningitis is serious and can be fatal within days without prompt antibiotic treatment. Delayed treatment increases the risk of permanent brain damage or death.
What to do if you suspect someone has meningitis?
Seek immediate medical care if you suspect that someone has meningitis. Early treatment of bacterial meningitis can prevent serious complications.
What is the term for inflammation of the membranes surrounding the brain and spinal cord?
Meningitis is an inflammation of the fluid and membranes (meninges) surrounding your brain and spinal cord.
How many people have died from vaping?
As mentioned before, at least 26 people in the United States have lost their lives because of their decision to vape. This number could be much higher, considering the likelihood that other people didn't report a history of vaping to their physicians. While more research clearly needs to be done regarding the potential health impact of vaping, the CDC strongly urges that you consider refraining from using e-cigarette, or vaping, products. For resources that can help you quit the use of vape products, visit the CDC's website here. And living your best healthy life can be simple with these 50 Secrets to Live to 100.
When did vaping start?
Vaping—meaning to the use of electronic cigarettes (or e-cigarettes), e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems—first debuted in 2003, and were marketed as a less-harmful alternative to smoking. A decade-and-a-half later, we are learning that isn't the case.
How many deaths from vaping have been confirmed?
Of those, 26 deaths have been confirmed in 21 states. While it is still unclear of the specific chemical exposure (s) causing these lung injuries associated with e-cigarette use, or vaping, all patients have reported a history of using e-cigarette, or vaping, products.
How old can you be if you vape?
It Can Age You. Akin to regular smoking, vaping can age you 10 years or more. "Vaping can age your skin similar to cigarettes," board-certified dermatologist Nazanin Saedi, MD, explains. "We know that people who smoke age prematurely, especially their skin.".
How many lung injuries are associated with vaping?
It Can Increase Your Chance of Lung Disease. Shutterstock. On October 10th, the CDC revealed that 1,299 lung injury cases associated with the use of e-cigarette, or vaping, products have been reported from 49 states, the District of Columbia, and one U.S. territory. Of those, 26 deaths have been confirmed in 21 states.
What are the chemicals in secondhand car exhaust?
They concluded that secondhand emissions contain, "nicotine; ultrafine particles; flavorings such as diacetyl, a chemical linked to serious lung disease; volatile organic compounds such as benzene, which is found in car exhaust; and heavy metals, such as nickel, tin, and lead.". 21.
Does vaping cause lung disease?
The CDC reports vaping is responsible for a mysterious lung disease, with the number of reported infections—and even deaths—increasing by the week. It's more important than ever to learn about the potential health risks. Eat This, Not That! Health spoke to several of the nation's top physicians and analyzed data from government agencies to discover 25 things vaping does to your body.

Overview
- Meningitis is an inflammation of the membranes (meninges) surrounding your brain and spinal cord.The swelling from meningitis typically triggers symptoms such as headache, fever and a stiff neck.Most cases of meningitis in the United States are caused by a viral infection, but bacterial, parasitic and fungal infections are other causes. Some cases of meningitis improve without trea…
- Meningitis is a condition that involves the inflammation of the lining of the brain, also called the meninges. It may be caused by a bacterial, fungal, or viral infection, which can develop into potentially fatal condition. Late diagnosis and treatment may result in permanent disability (such as hearing loss or brain damage), coma, or death. To prevent bacterial meningitis such as that a…
Causes
- Non-polio enteroviruses are the most common cause of viral meningitis in the United States, especially from late spring to fall. That is when these viruses spread most often. However, only a small number of people infected with enteroviruses will actually develop meningitis.Other viruses that can cause meningitis are 1. Mumps virus 2. Herpesviruses, including Epstein-Barr virus, her…
- Viral infections are the most common cause of meningitis, followed by bacterial infections and, rarely, fungal infections. Because bacterial infections can be life-threatening, identifying the cause is essential.
- It's for children and adults with sensorineural hearing loss. That condition typically involves damage to tiny hair cells in a part of your inner ear called the cochlea. These hair cells usually pick up the vibrations of sounds and send them to the brain through the auditory nerve. When theyre damaged, sound can't reach that nerve. A cochlear implant skips the damaged hair cells and sen…
- Meningitis has various causes, including bacterial infection (the most serious cases), viral infection, fungal infection, reactions to medications, and environmental toxins such as heavy metals. Although bacterial and fungal meningitis require extended hospitalization, meningitis caused by viruses can often be treated at home and has a much better outcome. Bacterial and v…
Signs And Symptoms
- 1. Fever 2. Irritability 3. Poor eating 4. Sleepiness or trouble waking up from sleep 5. Lethargy (a lack of energy)
- Early meningitis symptoms may mimic the flu (influenza). Symptoms may develop over several hours or over a few days.Possible signs and symptoms in anyone older than the age of 2 include: 1. Sudden high fever 2. Stiff neck 3. Severe headache that seems different than normal 4. Headache with nausea or vomiting 5. Confusion or difficulty concentrating 6. Seizures 7. Sleepin…
- The classic symptoms of meningitis are fever, headache, and stiff neck. Unfortunately, not everyone with meningitis has all of these symptoms. Only approximately 45% of people with meningitis have all three of these classic signs. Almost everyone, however, has at least one of the classic symptoms. Because meningitis can be so serious, seeking immediate medical care is es…
- The possible presence of bacterial meningitis is suggested by the symptoms of fever, altered mental status, headache, and nuchal rigidity. Although one or more of these findings are absent in many patients with bacterial meningitis [1-4], virtually all patients (99 to 100 percent) have at least one of the classic triad of fever, neck stiffness, and altered mental status [4]. (See \"Clinical feat…
Treatment
- In most cases, there is no specific treatment for viral meningitis. Most people who get mild viral meningitis usually recover completely in 7 to 10 days without treatment. Antiviral medicine may help people with meningitis caused by viruses such as herpesvirus and influenza.Antibiotics do not help viral infections, so they are not useful in the treatment of viral meningitis. However, anti…
- PRETREATMENT EVALUATION Antibiotic regimen There are three general requirements of antimicrobial therapy for bacterial meningitis [15]: Choice of regimen Antimicrobial selection must be empiric immediately after CSF is obtained or when lumbar puncture is delayed. In such patients, antimicrobial therapy needs to be directed at the most likely bacteria based upon patie…
- Initial empiric therapy of bacterial meningitis is based on the patient's age, risk factors, and clinical features (Table 1).3,4 In patients with suspected bacterial meningitis, empiric therapy should not be delayed for more than one hour while awaiting diagnostic testing or transfers.4,18,22,23 Although no prospective comparative trials have been performed, observati…
- Goals of treatment for meningitis in dogs include suppressing the inflammation, encouraging recovery from neurological conditions brought on by the disease, relieving pain, and controlling seizures. Treatment can vary depending on the cause of the inflammation. Most of the time treatment will usually begin with administration of steroids to suppress the immune system res…
Diagnosis
- Doctors diagnose meningitis by ordering specific lab tests on specimens from a person suspected of having meningitis. If a doctor suspects meningitis, he or she may collect samples for testing by: 1. Swabbing your nose or throat 2. Obtaining a stool sample 3. Taking some blood 4. Drawing fluid from around your spinal cord...
- The diagnosis of bacterial meningitis is discussed in greater detail separately. (See \"Clinical features and diagnosis of acute bacterial meningitis in adults\".)
- The diagnostic challenges in patients with clinical findings of meningitis are as follows: 1. Early identification and treatment of patients with acute bacterial meningitis 2. Assessing whether a treatable CNS infection is present in those with suspected subacute or chronic meningitis 3. Identifying the causative organism Blood studies that may be useful include the following: 1. Co…
- Your doctor will ask you questions about your symptoms and perform a physical exam. Your doctor will want to confirm the diagnosis by analyzing a sample of cerebrospinal fluid. Fluid is drawn through a needle from the lower part of the spinal cord in a procedure called a lumbar puncture (spinal tap). The fluid is then checked for the presence and type of bacteria. Knowing …
Prevention
- There are no vaccines to protect against non-polio enteroviruses, which are the most common cause of viral meningitis. The best way to help protect yourself and others from non-polio enterovirus infections is to 1. Wash your hands often with soap and water for at least 20 seconds, especially after changing diapers or using the toilet 2. Avoid close contact, such as touching an…
- Common bacteria or viruses that can cause meningitis can spread through coughing, sneezing, kissing, or sharing eating utensils, a toothbrush or a cigarette.These steps can help prevent meningitis: 1. Wash your hands. Careful hand-washing helps prevent the spread of germs. Teach children to wash their hands often, especially before eating and after using the toilet, spending ti…
- Avoidance of delay Antimicrobial therapy, along with adjunctive dexamethasone when indicated, should be initiated as quickly as possible after the performance of the lumbar puncture (LP) or, if a computed tomography (CT) scan of the head is to be performed before LP, as quickly as possible after blood cultures are obtained (algorithm 1) [5,9,11]. (See 'Pretreatment testing' abov…
- The infection that causes bacterial meningitis is treated with a combination of antibiotics. The antibiotics you receive will depend on the bacteria that are suspected, your age, and other factors. The antibiotics are injected into a vein. You might have to receive the antibiotics for as long as 3 weeks. For the first few days of antibiotic treatment, you may also be given dexamethasone* (a …
Complications
- Meningitis complications can be severe. The longer you or your child has the disease without treatment, the greater the risk of seizures and permanent neurological damage, including: 1. Hearing loss 2. Memory difficulty 3. Learning disabilities 4. Brain damage 5. Gait problems 6. Seizures 7. Kidney failure 8. Shock 9. DeathWith prompt treatment, even patients with severe me…
- The severity of complications generally increases with the severity of the original infection. A study of teens that survived meningitis infection found that more than half had physical aftereffects. Symptoms may include: 1. partial or total hearing loss 1. memory and concentration problems 2. balance and coordination problems 3. temporary or permanent learning difficulties …
- Complications of patients with bacterial meningitis include: 1. Visual impairment. Infection may spread towards the eyes if left untreated. 2. Deafness. Deafness may also occur when the bacteria reaches the optic nerve. 3. Seizures. The bacteria irritates the meningeal layers and may lead to seizures.
- 1. Immediate: septic shock, including disseminated intravascular coagulation, coma with loss of protective airway reflexes, cerebral oedema and raised intracranial pressure, septic arthritis, pericardial effusion and haemolytic anaemia (H. influenzae). 2. Subdural effusions are a common complication in young children. Risk factors include young age, rapid onset of illness, low periph…
Prognosis
- INTRODUCTION Bacterial meningitis is a medical emergency, and immediate steps must be taken to establish the specific cause and initiate effective therapy. The mortality rate of untreated disease approaches 100 percent, and, even with optimal therapy, there is a high failure rate. Duration The duration of antimicrobial therapy for bacterial meningitis depends upon the causati…
- The mortality rate in adults with bacterial meningitis in developed countries is 21 percent; it is higher in patients with pneumococcal disease than in those with meningococcal disease.7 Neurologic sequelae include hearing loss in 14 percent of patients and hemiparesis in 4 percent.7 Risk factors for adverse outcomes include advanced age, alteration of mental status on admissi…
- The likelihood of recovery can vary depending on the cause of the meningitis and how far it has progressed. For infections that have reached the central nervous system, the prognosis is not favorable. Sadly, many dogs die from these types of infections. Dogs responses to treatment, however, can vary greatly, and early and aggressive medical intervention always improves the od…
People At Risk
- People of any age can get viral meningitis. However, some people have a higher risk of getting the disease, including: 1. Children younger than 5 years old 2. People with weakened immune systems caused by diseases, medications (such as chemotherapy), and recent organ or bone marrow transplantationsBabies younger than 1 month old and people with weakened immune systems a…
- Risk factors for meningitis include: 1. Skipping vaccinations. Risk rises for anyone who hasn't completed the recommended childhood or adult vaccination schedule. 2. Age. Most cases of viral meningitis occur in children younger than age 5. Bacterial meningitis is common in those under age 20. 3. Living in a community setting. College students living in dormitories, personnel on mili…
Epidemiology
- No known immune deficiency S. pneumoniae, N. meningitidis, and, less often, H. influenzae and group B Streptococcus are the most likely causes of community-acquired bacterial meningitis in otherwise healthy adults up to the age of 60 years [31]. Individuals over aged 50 years are also at increased risk of L. monocytogenes meningitis [32]. (See \"Epidemiology of bacterial meningitis …
- 1. The annual incidence of acute bacterial meningitis in developed countries is estimated to be 1-2 per 100,000. 2. Public Health England publishes annual reports on laboratory-confirmed invasive meningococcal disease. In the epidemiological year (start of July to end of June) 2017-2018 there were 755 confirmed cases in England, similar to the 748 cases reported in 2016-2017. 3. Tables …
- Overall, rash is not unusual in those with meningitis but can be particularly symbolic for meningococcal meningitis. For instance, in one study of patients with meningitis caused by a bacteria, rash occurred 26 percent and of those with a rash, 92 percent were associated with meningococcal meningitis. Please remember, though, an individual can have petechiae and NO…